









|
Hurler's Syndrome (Mucopolysaccharidosis
I) Hurler, Scheie and
Hurler/Scheie syndromes are mucopolysaccharide disorders and are also known
respectively as MPS-IH, MPS-IS, and MPS-IH/S. Hurler syndrome takes its name
from Gertrud Hurler, the doctor who described a boy and girl with the
condition in 1919. In 1962, Dr. Scheie, a consultant ophthalmologist, wrote
about some of his patients who were more mildly affected. Patients who seem
not to fit clearly in either the severe or the mild end of the disorder are
said to have Hurler/Scheie syndrome.
There is no magic cure for MPS disorders, but there are ways of managing and
treating the problems they cause.
What Causes the Disorder?
Mucopolysacchrides are
long chains of sugar molecule used in the building of connective tissues in
the body.
"saccharide" is a general
term for a sugar molecule (think of saccharin)
"poly" means many
"muco"
refers to the thick
jelly-like consistency of the molecules
There is a continuous
process in the body of replacing used materials and breaking them down for
disposal. Children with these disorders are missing an enzyme called
alpha-L-iduronidase which is essential in cutting up the mucopolysaccharides
called dermatan and heparan sulfate. The incompletely broken down
mucopolysaccharides remain stored in cells in the body causing progressive
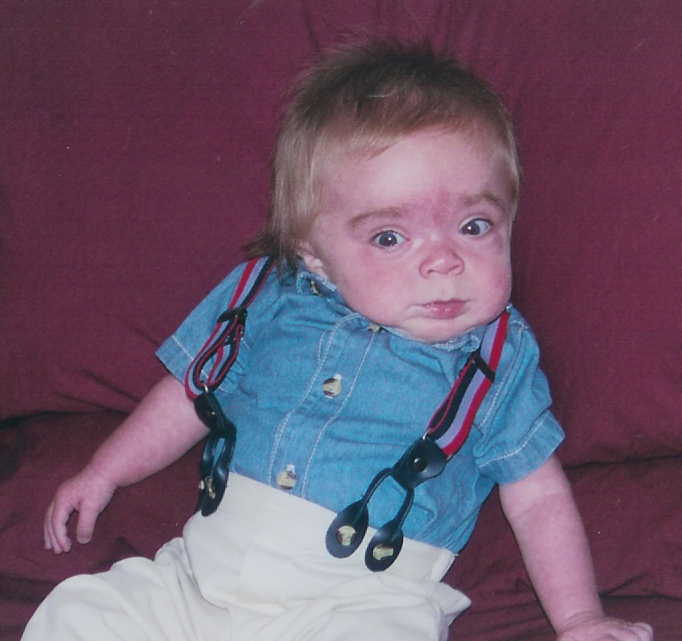
damage. Babies may show little sign of the disorder, but as more and more
cells become damaged, symptoms start to appear.

How Common is the Disorder?
Estimations
1 in 100,000 babies born would have
Hurler syndrome.
Scheie syndrome is 1 in
500,000
Hurler/Scheie syndrome it is 1 in 115,000.
There is an estimate in the United States that 1 in 25,000 births will
result in some form of MPS. Other estimates state only 40 babies a year are
born with Hurlers.
How is the Disorder Inherited?
We all have genes inherited from our
parents which control whether we are tall, short, fair, etc. Some genes we
inherit are "recessive," that is to say we carry the gene, but it does not
have any affect on our development. Hurler syndrome is caused by a recessive
gene. If an adult carrying the abnormal gene marries another carrier, there
will be a one in four chance with every pregnancy that the child will
inherit the defective gene from each parent and will be affected with the
disorder. There is a two in three chance that unaffected brothers and
sisters of MPS I children will be carriers. They can be reassured; however,
that, as the disorder is so rare, the chance of marrying another carrier is
very slight provided they do not marry a cousin or other close family
member. However, you can not find two more different genetic background's
than Joe and I. His family is all from Italy, and I like to say, I am 100%
blond!!!!
Layman's Explanation
The disorder is based on the bodies
inability to produce a specific enzyme that is used to breakdown cellular
byproducts into other molecules the body can use. These molecules
build up in the body and are stored in the cells where they were originally
used. Over time these molecules begin to get in the way and cause a
slow down in the normal cellular processes that take place in the body.
The most common effects of this build up are mental deficiencies, skeletal
and joint problems, vision and hearing impairment, heart, liver and lung
disease. The end result is death.
Current Treatment Options
There are many treatment options
available for Hurler's.
- Enzyme Replacement Therapy -
Introduction of the missing enzyme back into the body through a central
line or peripheral line.
Transplantation options:
- Bone Marrow Transplants - Complete
obliteration of the Childs malfunctioning bone marrow and replacement with
healthy bone marrow that can produce the needed enzyme
- Stem Cell Transplants
- Introduction
of stem cells into the body which produce the required cells in the
treated organ to create the enzyme
- Umbilical Cord
Transplants:
 |
In the 1970s medical
researchers discovered that human umbilical cord blood contained the
same kind of stem cells found in bone marrow. (Stem cells get their
name from their ability to develop into three types of blood cells:
red blood cells, while blood cells and platelets). Because stem
cells from bone marrow had already been used successfully to treat
patients with life-threatening blood diseases, such as leukemia and
immune system disorders, researchers believed that they could also
use stem cells from cord blood to save patients.
In 1988, doctors transplanted human umbilical cord blood into a
5-year old boy suffering from Fanconi's anemia. Ten years after the
transplant, the boy is alive and seems to be cured of his disease.
Based on this and other successful transplants, doctors and medical
researchers began to collect, freeze and store cord blood units (CBUs)
at cord banks throughout the world. As of October 1998, there were
approximately 22,000 CBUs collected and frozen for use worldwide,
and approximately 700 unrelated donor and 150 related (sibling)
donor cord blood transplants had been performed.
Although today marrow transplants and cord blood transplants are
often referred to by the same name -- stem cell transplants -- there
are important differences between the two. This section will explain
these differences and also discuss the kinds of decisions doctors
and their patients must make to determine the best source of stem
cells for transplantation. Before considering these issues, however,
it is important to understand the challenges patients face in
finding a donor.
Unfortunately, 70% of patients who need a stem cell transplant do
not have a suitable donor in their family. The National Marrow Donor
Program (NMDP) helps identify stem cell donors for patients who do
not have a related donor.
Stem cell transplants require matching certain tissue traits of
the donor and patient. Because these traits are inherited, a
patient's most likely match is someone of the same heritage.
American Indian and Alaska Native, Asian, Black and African
American, Hispanic and Latino, Native Hawaiian and Other Pacific
Islander, and multiple-race patients face a greater challenge in
finding a match than White patients.
The collection and storage of cord blood is one way to give
patients of all racial and ethnic backgrounds greater access to stem
cell transplantation. For that reason, beginning in the early to
mid-1990s, medical institutions around the world began making a
serious effort to collect and store cord blood units for use in
transplantation.
So far, clinical studies by John E. Wagner and others suggest
that unrelated cord blood transplantation is a safe and acceptable
alternative to bone marrow transplantation for many patients.
However, these studies have also found that, as with bone marrow
transplants, patients who receive cord blood from sibling (or
related) donors generally have higher survival rates than those who
receive cord blood from unrelated donors.
Studies have also found that banked cord blood (from both related
and unrelated donors) often contains enough stem cells for
transplantation. Physicians need to match the number of stem cells
in a cord blood unit with the weight of the patient to be sure the
unit is likely to be able to reestablish the patient's immune
system. Because there are fewer stem cells in cord blood than in
marrow, until recently most cord blood recipients have been children
or small adults. There is, therefore, some concern that the number
of cells in an average cord blood unit may not be sufficient for
engraftment in larger adults. Engraftment occurs when the
transplanted stem cells -- the "graft" -- regenerate the blood and
marrow and begin to function as the recipient's new immune system.
One positive finding is that cord blood transplant patients
appear to suffer less from acute
graft-versus-host disease (GVHD)
than patients who receive bone marrow transplants. GVHD is a very
serious, and sometimes fatal, condition that occurs when the
patient's new immune system -- which is made up of stem cells from
the donor -- starts attacking the patient's body. GVHD affects the
skin and internal organs such as the liver and intestines.
Despite the fact that cord blood recipients appear to suffer less
from GVHD, it has not yet been proven that the risk of GVHD is less
in all recipients after cord blood transplantation. Because
children receive the most cord blood transplants, and because they
also experience less GVHD than adults after bone marrow transplants,
it may be that the success of cord blood transplants is at least
partly attributable to the fact that they are used on more children
than adults.
With stem cell transplants, the better the match between the
donor and the recipient, the less likely graft-versus-host disease
is to develop. It is important, therefore, to understand how doctors
determine the best, or most acceptable, match between the donor and
the recipient. To understand how they do this, it helps to have a
basic understanding of the human immune system.
Antigens, a kind of protein located on the outer surface of most
cells in the body, help the immune system to identify foreign
bacteria and viruses. The antigens that transplant doctors look for
when matching patients and donors are located on a cell called a
leukocyte, giving these antigens the name
Human Leukocyte Antigens, or HLA. Every person has six groups
of HLA antigens, but three groups (called A, B, and DR) are
considered most important in a stem cell transplant. Each of these
groups has two antigens, one inherited from the father and one from
the mother, making a total of six antigens that determine a
donor/recipient match. A perfect match is
called a 6/6 HLA match.
Bone marrow transplants are usually not attempted unless the
donor and recipient are a 6/6 or 5/6 HLA match. However, with cord
blood transplants, doctors and medical researchers generally believe
that a 4/6 match is sufficient. Because immune system cells
contained in cord blood are less mature, they have not yet "learned"
to attack foreign substances, and so would be less likely to attack
the recipient's immune system, even though the match isn't perfect.
Since matching requirements for cord blood are less strict, patients
who are unable to find a 5/6 or 6/6 marrow donor may be able to find
a suitably matched cord blood unit.
With its more than 30-year history, bone marrow transplants are a
well-established, life-saving treatment for a wide range of blood
disorders such as leukemia and aplastic anemia, as well as selected
immune system deficiencies and genetic disorders. While the history
of cord blood transplants is less extensive, there is evidence to
suggest that these transplants can cure diseases, too. But with cord
blood there are more unknowns, and doctors and their patients must
carefully evaluate the situation before deciding on the best
treatment.
The following lists explain what is known and not known about
cord blood transplants. While these lists are not exhaustive, they
do include aspects of cord blood transplants that are critical in
the decision-making process:
- Cord blood contains sufficient numbers
of stem cells for engraftment in most recipients weighing less
than 50 kilograms (about 110 pounds).
- Collection of cord blood poses no
health risk to the mother or infant donor.
- Because it is stored and available for
use, cord blood is sometimes more readily available than a
potential marrow or blood stem donor, who may be unavailable for
donation when it is needed.
- Cord blood is rarely contaminated by
viruses often found in marrow, such as cytomegalovirus (CMV) and
Epstein-Barr virus.
- Cord blood can cause severe GVHD, but
possibly less frequently than in bone marrow transplants.
- Compared to bone marrow transplants,
cord blood transplants may have a lower rate of acute GVHD, at
least in cases where a related (sibling) donor is used.
- It appears that the transplant process
using cord blood (from the time a search is started to the time
donor cells are ready for transplant) is shorter than that for
marrow cell donation because the cord blood units are in storage
and ready for use.
- Whether cord blood is sufficient for
engraftment in most adult recipients, although experience
suggests that it may be sufficient for a significant proportion
of these recipients.
- Whether cord blood transplants pose a
different risk of relapse (recurrence of an illness after a
remission) compared to unrelated bone marrow transplants.
- Whether focused cord blood collection
will be successful in meeting the current challenge of finding a
match for American Indian and Alaska Native, Asian, Black and
African American, Hispanic and Latino, Native Hawaiian and Other
Pacific Islander, and multiple-race patients, thus increasing
the number of available transplants for these patients.
Clinical studies have demonstrated that
stored cord blood is a sufficient source of transplantable stem
cells, at least for young patients. Also, in addition to
previously known advantages of cord blood (rapid availability and a
low rate of virus contamination) studies have found that cord blood
transplants may also lead to less GVHD than bone marrow transplants.
Clinical experience also shows that a high stem cell dose (a
sufficient number of stem cells based on the patient's body weight)
is an important factor in recipient survival, and that cord blood
transplants can be successful with as low as a 4/6 HLA match.
*Visit "Chemo Counting" to see what a
typical hospital day will include* |
| |
|
Graph Versus Host Disease (GVHD)
GVHD is a frequent complication of an unrelated bone marrow or umbilical
chord transplant. The transplanted cells realize that they are in a
new environment and attack the donor's organs. Approximately 50% of
patients that receive an unrelated transplant contract GVHD, the numbers are
less in umbilical chord transplants at 25%. There are two types of
GVHD, acute and chronic. Acute GVHD occurs soon after the transplant
between day 30 and day 60. Chronic GVHD can occur much later after
transplant and last much longer. Both types of GVHD can be serious and
range from level 1 through level 4 where level 4 is the most severe.
Most patients that contract GVHD are treated with steroids and a variety of
anti-rejection medications. The disorder has no long term side effects
if treated properly.
T-Cells are the cells in the transplanted marrow that recognize foreign
matter. Their sole purpose is to fight off infections, viruses, and
other foreign substances. These T-Cells look for genetic markers, HLA
markers, that distinguish them from foreign cells. To T-Cells normal
body cells can be foreign and are therefore considered bad. The
T-Cells will fight these cells trying to rid the body of them.
Obviously these small amount of T-Cells are not going to kill the entire
human body but the side effects of GVHD can be uncomfortable. Typical
side effects are diarrhea, rashes, increased liver functions, stomach and
intestinal problems.
**Information obtained from MPS website,
and National Marrow Donor Program |











